Medi Services

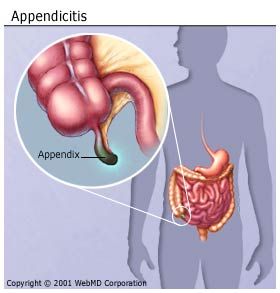
Appendicitis is inflammation of the appendix. Appendicitis commonly presents with right lower abdominal pain, nausea, vomiting, and decreased appetite.[2]However, one third to a half of persons do not have these typical signs and symptoms.[3] Severe complications of a ruptured appendix include widespread, painful inflammation of the inner lining of the abdominal wall and sepsis.[4]
Appendicitis is caused by a blockage of the hollow portion of the appendix,[5][6] most commonly by a calcified "stone" made of feces. However, inflamedlymphoid tissue from a viral infection, parasites, gallstone, or tumors may also cause the blockage.[7] This blockage leads to increased pressures within the appendix, decreased blood flow to the tissues of the appendix, and bacterial growth inside the appendix causing inflammation.[7][8] The combination of inflammation, reduced blood flow to the appendix and distention of the appendix causes tissue injury and tissue death.[9] If this process is left untreated, the appendix may burst, releasing bacteria into the abdominal cavity, leading to severe abdominal pain and increased complications.[9][10]
The diagnosis of appendicitis is largely based on the person's signs and symptoms.[8] In cases where the diagnosis cannot be made based on the person's history and physical exam, close observation, radiographic imaging and laboratory tests can often be helpful.[11] The two most common imaging tests used areultrasound and computed tomography (CT scan).[11] CT scan has been shown to be more accurate than ultrasound in detecting acute appendicitis.[12] However, ultrasound may be preferred as the first imaging test in children and pregnant women because of the risks associated with radiation exposure from CT scans.[11]
The standard treatment for acute appendicitis is surgical removal of the appendix.[7][8] This may be done by an open incision in the abdomen (laparotomy) or through a few smaller incisions with the help of cameras (laparoscopy). Surgery decreases the risk of side effects or death associated with rupture of the appendix.[4] Antibiotics may be equally effective in certain cases of non-ruptured appendicitis.[13] It is one of the most common and significant causes of severe abdominal pain that comes on quickly worldwide. In 2013 about 16 million cases of appendicitis occurred.[14] This resulted in 72,000 deaths globally.[15]In the United States, appendicitis is the most common cause of acute abdominal pain requiring surgery.[2] Each year in the United States, more than 300,000 persons with appendicitis have their appendix surgically removed.[16] Reginald Fitz is credited with being the first person to describe the condition in a paper published in 1886.[17]
Appendicitis is a medical emergency that requires prompt surgery to remove the appendix. Left untreated, an inflamed appendix will eventually burst, or perforate, spilling infectious materials into the abdominal cavity. This can lead to peritonitis, a serious inflammation of the abdominal cavity's lining (the peritoneum) that can be fatal unless it is treated quickly with strong antibiotics.
The presentation of acute appendicitis includes abdominal pain, nausea, vomiting, and fever. As the appendix becomes more swollen and inflamed, it begins to irritate the adjoining abdominal wall. This leads to the localization of the pain to the right lower quadrant. This classic migration of pain may not be seen in children under three years. This pain can be elicited through various signs and can be severe. Signs include localized findings in the right iliac fossa. The abdominal wall becomes very sensitive to gentle pressure (palpation). Also, there is severe pain on sudden release of deep pressure in the lower abdomen (rebound tenderness). If the appendix is retrocecal (localized behind the cecum), even deep pressure in the right lower quadrant may fail to elicit tenderness (silent appendix). This is because the cecum, distended with gas, protects the inflamed appendix from pressure. Similarly, if the appendix lies entirely within the pelvis, there is usually complete absence of abdominal rigidity. In such cases, a digital rectal examination elicits tenderness in the rectovesical pouch. Coughing causes point tenderness in this area (McBurney's point).
Acute appendicitis seems to be the end result of a primary obstruction of the inside (lumen) of the appendix.[5][6] Once this obstruction occurs, the appendix becomes filled with mucus and swells. This continued production of mucus leads to increased pressures within the lumen and the walls of the appendix. This increased pressure results in thrombosis and occlusion of the small vessels, and stasis of lymphatic flow. At this point spontaneous recovery rarely occurs. As the occlusion of blood vessels progresses, the appendix becomes ischemic and then necrotic. As bacteria begin to leak out through the dying walls, pus forms within and around the appendix (suppuration). The end result of this cascade is appendiceal rupture (a 'burst appendix') causing peritonitis, which may lead to sepsis and eventually death. This cascade of events is responsible for the slowly evolving abdominal pain and other commonly associated symptoms.[9]
The causative agents include bezoars, foreign bodies, trauma, intestinal worms, lymphadenitis, and, most commonly, calcified fecal deposits that are known as appendicoliths or fecaliths.[18][19] The occurrence of obstructing fecaliths has attracted attention since their presence in persons with appendicitis is higher in developed than in developing countries.[20] In addition an appendiceal fecalith is commonly associated with complicated appendicitis.[21] Also, fecal stasis and arrest may play a role, as demonstrated by persons with acute appendicitis having fewer bowel movements per week compared with healthy controls.[19][22]
The occurrence of a fecalith in the appendix was thought to be attributed to a right-sided fecal retention reservoir in the colon and a prolonged transit time. However, a prolonged transit time was not observed in subsequent studies.[23] From epidemiological data, it has been stated that diverticular disease and adenomatous polyps were unknown and colon cancer exceedingly rare in communities exempt from appendicitis.[24][25] Also, acute appendicitis has been shown to occur antecedent to cancer in the colon and rectum.[26]Several studies offer evidence that a low fiber intake is involved in the pathogenesis of appendicitis.[27][28][29] This low intake of dietary fiber is in accordance with the occurrence of a right-sided fecal reservoir and the fact that dietary fiber reduces transit time.[30]
Diagnosis is based on a medical history (symptoms) and physical examination which can be supported by an elevation of neutrophilic white blood cells and imaging studies if needed. (Neutrophils are the primary white blood cells that respond to a bacterial infection.) Histories fall into two categories, typical and atypical. Typical appendicitis includes several hours of generalized abdominal pain which begins in the region of the umbilicus with associated anorexia, nausea, or vomiting. The pain then "localizes" into the right lower quadrant where the tenderness increases in intensity. However, it is possible the pain could localize to the left lower quadrant in persons with situs inversus totalis. The combination of pain, anorexia, leukocytosis, and fever is classic. Atypical histories lack this typical progression and may include pain in the right lower quadrant as an initial symptom. Irritation of the peritoneum (inside lining of the abdominal wall) can lead to increased pain on movement, or jolting, for example going over speedbumps.[31] Atypical histories often require imaging with ultrasound and/or CT scanning.[32]
While there is no laboratory test specific for appendicitis, a complete blood count (CBC) is done to check for signs of infection. Although 70-90 percent of people with appendicitis may have an elevated white blood cell (WBC) count, there are many other abdominal and pelvic conditions that can cause the WBC count to be elevated.[35]
A urinalysis generally does not show infection but it is important for determining pregnancy status, especially the possibility of an ectopic pregnancy in woman of childbearing age. The urinalysis is also important for ruling out a urinary tract infection as the cause of abdominal pain. The presence of more than 20 WBC per high-power field in the urine is more suggestive of a urinary tract disorder.[35]
In children the clinical examination is important for determination of which children with abdominal pain should receive immediate surgical consultation and which should receive diagnostic imaging.[36]Because of the health risks of exposing children to radiation, ultrasound is the preferred first choice with CT-scan being a legitimate follow-up if the ultrasound is inconclusive.[37][38][39] CT scan is more accurate than ultrasound for the diagnosis of appendicitis in adults and adolescents. CT scan has a sensitivity of 94%, specificity of 95%. Ultrasonography had an overall sensitivity of 86%, a specificityof 81%.[40]
Ultrasonography and Doppler sonography provide useful means to detect appendicitis, especially in children. Ultrasound can also show free fluid collection in the right iliac fossa, along with a visible appendix without blood flow when using color Doppler, and noncompressibility of the appendix, as it is essentially a walled off abscess. In some cases (15% approximately), however, ultrasonography of the iliac fossa does not reveal any abnormalities despite the presence of appendicitis. This false negative finding is especially true of early appendicitis before the appendix has become significantly distended. In addition false negative findings are more common in adults where larger amounts of fat and bowel gas make visualizing the appendix technically difficult. Despite these limitations, sonographic imaging in experienced hands can often distinguish between appendicitis and other diseases with similar symptoms. Some of these conditions include inflammation of lymph nodes near the appendix or pain originating from other pelvic organs such as the ovaries or fallopian tubes.
Where it is readily available, computed tomography (CT) has become frequently used, especially in people whose diagnosis is not obvious on history and physical examination. Concerns about radiation, however, tend to limit use of CT in pregnant women and children, especially with the increasingly widespread usage of MRI.[41][42]
The accurate diagnosis of appendicitis is multi-tiered, with the size of the appendix having the strongest positive predictive value, while indirect features can either increase or decrease sensitivity and specificity. A size of over 6 mm is both 95% sensitive and specific for appendicitis.[43]
However, because the appendix can be filled with fecal material, causing intraluminal distention, this criterion has shown limited utility in more recent meta analyses.[44] This is as opposed to ultrasound, in which the wall of the appendix can be more easily distinguished from intraluminal feces. In such scenarios, ancillary features such as increased wall enhancement as compared to adjacent bowel, and inflammation of the surrounding fat, or fat stranding, can be supportive of the diagnosis, although their absence does not preclude it. In severe cases with perforation, an adjacent phlegmon or abscess can be seen. Dense fluid layering in the pelvis can also result, related to either pus or enteric spillage. When patients are thin or younger, the relative absence of fat can make both the appendix and surrounding fat stranding difficult to see.[44]
MRI usage has become increasingly common for diagnosis of appendicitis in children and pregnant patients due to the radiation dosage that, while of nearly negligible risk in healthy adults, can be harmful to children or the developing fetus. In pregnancy, it has been found to be more useful during the second and third trimester, particularly as the enlargening uterus displaces the appendix, making it difficult to find by ultrasound. The periappendiceal stranding that is reflected on CT by fat stranding on MRI appears as increased fluid signal on T2 weighted sequences. First trimester pregnancies are usually not candidates for MRI, as the fetus is still undergoing organogenesis, and there are no long term studies to date regarding its potential risks or side effects.[45]
In general, plain abdominal radiography (PAR) is not useful in making the diagnosis of appendicitis and should not be routinely obtained in a person being evaluated for appendicitis.[46][47] Plain abdominal films may be useful for the detection of ureteral calculi, small bowel obstruction, or perforated ulcer, but these conditions are rarely confused with appendicitis.[48] An opaque fecalith can be identified in the right lower quadrant in less than 5% of persons being evaluated for appendicitis.[35] Abarium enema has proven to be a poor diagnostic tool for appendicitis. While failure of the appendix to fill during a barium enema has been associated with appendicitis, up to 20% of normal appendices also do not fill.[48]
| Migratory right iliac fossa pain | 1 point |
| Anorexia | 1 point |
| Nausea and vomiting | 1 point |
| Right iliac fossa tenderness | 2 points |
| Rebound abdominal tenderness | 1 point |
| Fever | 1 point |
| High white blood cell count (leukocytosis) | 2 points |
| Shift to left (segmented neutrophils) | 1 point |
| Total score | 10 points |
|---|
No excellent scoring system exists to determine if a child has appendicitis.[49] The Alvarado score and pediatric appendicitis score are okay but not definitive.[49]
The Alvarado score is the most widely used scoring system. A score below 5 suggests against a diagnosis of appendicitis, whereas a score of 7 or more is predictive of acute appendicitis. In a person with an equivocal score of 5 or 6, a CT scan or ultrasound exam may be used to reduce the rate of negative appendectomy.
The definitive diagnosis is based on pathology. The histologic finding of appendicitis is neutrophilic infiltrate of the muscularis propria.
Periappendicits, inflammation of tissues around the appendix, is often found in conjunction with other abdominal pathology.[50]
Children: Gastroenteritis, mesenteric adenitis, Meckel's diverticulitis, intussusception, Henoch-Schönlein purpura, lobar pneumonia, urinary tract infection (abdominal pain in the absence of other symptoms can occur in children with UTI), new-onset Crohn's disease or ulcerative colitis, pancreatitis, and abdominal trauma from child abuse; distal intestinal obstruction syndrome in children with cystic fibrosis; typhlitis in children with leukemia.
Women: A pregnancy test is important in all women of childbearing age since an ectopic pregnancy can have signs and symptoms similar to those of appendicitis. Other obstetrical/gynecological causes of similar abdominal pain in women include pelvic inflammatory disease, ovarian torsion, menarche, dysmenorrhea,endometriosis, and Mittelschmerz (the passing of an egg in the ovaries approximately two weeks before an expected menstruation cycle).[51]
Men: testicular torsion;
Adults: new-onset Crohn's disease, ulcerative colitis, regional enteritis, renal colic, perforated peptic ulcer, pancreatitis, rectus sheath hematoma and epipliocitis.
Elderly: diverticulitis, intestinal obstruction, colonic carcinoma, mesenteric ischemia, leaking aortic aneurysm.
The term "pseudoappendicitis" is used to describe a condition mimicking appendicitis.[52] It can be associated with Yersinia enterocolitica.[53]
Sometimes a pus-filled abscess (infection that is walled off from the rest of the body) forms outside the inflamed appendix. Scar tissue then "walls off" the appendix from the rest of the abdomen, preventing infection from spreading. An abscessed appendix is a less urgent situation, but unfortunately, it can't be identified without surgery. For this reason, all cases of appendicitis are treated as emergencies, requiring surgery.
Appendicitis occurs when the appendix becomes blocked, often by stool, a foreign body, or cancer. Blockage may also occur from infection, since the appendix swells in response to any infection in the body.
What Are the Symptoms of Appendicitis?
The classic symptoms of appendicitis include:
Almost half the time, other symptoms of appendicitis appear, including:
If you have any of the mentioned symptoms, seek medical attention immediately, because timely diagnosis and treatment is very important. Do not eat, drink, or use any pain remedies, antacids, laxatives, or heating pads, which can cause an inflamed appendix to rupture.
How Is Appendicitis Diagnosed?
Diagnosing appendicitis can be tricky. Symptoms of appendicitis are frequently vague or extremely similar to other ailments, includinggallbladder problems, bladder orurinary tract infection, Crohn's disease, gastritis, intestinal infection, and ovary problems.
The following tests are usually used to make the diagnosis: