Medi Services

Meningitis is a relatively rare infection that affects the delicate membranes -- called meninges (men-in'-jeez) -- that cover the brain and spinal cord. Bacterial meningitis can be deadly and contagious among people in close contact.
Viral meningitis tends to be less severe and most people recover completely without specific therapy.
Fungal meningitis is a rare form of meningitis and generally occurs only in people with weakened immune systems.Meningitis is an acute inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges.[1] The most common symptoms are fever, headache and neck stiffness. Other symptoms include confusion or altered consciousness, vomiting, and an inability to tolerate light or loud noises. Young children often exhibit only nonspecific symptoms, such as irritability, drowsiness, or poor feeding.[2] If a rash is present, it may indicate a particular cause of meningitis; for instance, meningitis caused by meningococcal bacteria may be accompanied by a characteristic rash.[1][3]
The inflammation may be caused by infection with viruses, bacteria, or other microorganisms, and less commonly by certain drugs.[4] Meningitis can be life-threatening because of the inflammation's proximity to the brain and spinal cord; therefore, the condition is classified as a medical emergency.[1][5] A lumbar puncture diagnoses or excludes meningitis.[2] A needle is inserted into the spinal canal to collect a sample of cerebrospinal fluid (CSF), that envelops the brain and spinal cord. The CSF is examined in a medical laboratory.[5]
Some forms of meningitis are preventable by immunization with the meningococcal, mumps, pneumococcal, and Hib vaccines.[1] Giving antibiotics to people with significant exposure to certain types of meningitis may also be useful.[2] The first treatment in acute meningitis consists of promptly giving antibiotics and sometimes antiviral drugs.[2][6] Corticosteroids can also be used to prevent complications from excessive inflammation.[3][5] Meningitis can lead to serious long-term consequences such as deafness, epilepsy, hydrocephalus, or cognitive deficits, especially if not treated quickly.[1][3]
Meningitis is almost always caused by a bacterial or viral infection that began elsewhere in the body, such as in the ears, sinuses, or upper respiratory tract. Less common causes of meningitis include fungal infection, autoimmune disorders, and medications.
Bacterial Meningitis
Bacterial meningitis is an extremely serious illness that requires immediate medical care. If not treated quickly, it can lead to death within hours -- or lead to permanent damage to the brain and other parts of the body.
Bacterial meningitis is caused by any one of several bacteria. The most common bacteria causing meningitis in children and adults in the U.S. are Neisseria meningitidis ("meningococcus"), Streptococcuspneumoniae("pneumococcus") and, in older patients with decreased immunity,Listeria monocytogenes. Haemophilus influenzae type b (Hib) was a common cause of meningitis in infants and young children until the Hib vaccine was introduced for infants. Vaccines are available for bothNeisseria meningitidis and Streptococcus pneumoniae. They're recommended for all children and adults at special risk.
The bacteria can spread from person to person through coughing andsneezing. If you are around someone who has bacterial meningitis, contact your health care provider to ask what steps you need to take to avoid infection.
In many instances, bacterial meningitis develops when bacteria get into the bloodstream from the sinuses, ears, or other part of the upper respiratory tract. The bacteria then travel through the bloodstream to the brain.
Viral Meningitis
Viral meningitis is more common than the bacterial form and generally -- but not always -- less serious. It can be triggered by a number of viruses, including several that can cause diarrhea.
People with viral meningitis are much less likely to have permanentbrain damage after the infection resolves. Most will recover completely.
Fungal Meningitis
Fungal meningitis is much less common than the other two infectious forms. Fungus-related meningitis is rare in healthy people. However, someone who has an impaired immune system -- such as a person with AIDS -- is more likely to become infected with this form of meningitis.
Who Is Most at Risk for Meningitis?
Anyone can develop just about any kind of meningitis. But research has shown that some age groups have higher rates of meningitis than others. They are:
Studies have shown that meningitis is more of a danger for people with certain medical conditions, such as a damaged or absent spleen, chronic disease, or immune system disorders.
Because certain germs that cause meningitis can be contagious, outbreaks are most likely to occur in places where people are living in close quarters. So college students in dorms or army recruits in barracks are at higher risk. So are people traveling to areas where meningitis is more common, such as parts of Africa.
However, keep this in mind. Even if your personal odds of getting meningitis are higher than average, it's still a rare disease and there are steps you can take to minimize your risk of getting the disease.
In adults, the most common symptom of meningitis is a severe headache, occurring in almost 90% of cases of bacterial meningitis, followed by nuchal rigidity (the inability to flex the neck forward passively due to increased neck muscle tone and stiffness).[12] The classic triad of diagnostic signs consists of nuchal rigidity, sudden high fever, and altered mental status; however, all three features are present in only 44–46% of bacterial meningitis cases.[12][13] If none of the three signs are present, acute meningitis is extremely unlikely.[13] Other signs commonly associated with meningitis include photophobia (intolerance to bright light) andphonophobia (intolerance to loud noises). Small children often do not exhibit the aforementioned symptoms, and may only be irritable and look unwell.[1] Thefontanelle (the soft spot on the top of a baby's head) can bulge in infants aged up to 6 months. Other features that distinguish meningitis from less severe illnesses in young children are leg pain, cold extremities, and an abnormal skin color.[14][15]
Nuchal rigidity occurs in 70% of bacterial meningitis in adults.[13] Other signs of meningism include the presence of positive Kernig's sign or Brudzi?ski sign. Kernig's sign is assessed with the person lying supine, with the hip and knee flexed to 90 degrees. In a person with a positive Kernig's sign, pain limits passive extension of the knee. A positive Brudzinski's sign occurs when flexion of the neck causes involuntary flexion of the knee and hip. Although Kernig's sign and Brudzinski's sign are both commonly used to screen for meningitis, the sensitivity of these tests is limited.[13][16] They do, however, have very good specificity for meningitis: the signs rarely occur in other diseases.[13] Another test, known as the "jolt accentuation maneuver" helps determine whether meningitis is present in those reporting fever and headache. A person is asked to rapidly rotate the head horizontally; if this does not make the headache worse, meningitis is unlikely.[13]
Meningitis caused by the bacterium Neisseria meningitidis (known as "meningococcal meningitis") can be differentiated from meningitis with other causes by a rapidly spreading petechial rash, which may precede other symptoms.[14] The rash consists of numerous small, irregular purple or red spots ("petechiae") on the trunk, lower extremities, mucous membranes, conjuctiva, and (occasionally) the palms of the hands or soles of the feet. The rash is typically non-blanching; the redness does not disappear when pressed with a finger or a glass tumbler. Although this rash is not necessarily present in meningococcal meningitis, it is relatively specific for the disease; it does, however, occasionally occur in meningitis due to other bacteria.[1] Other clues on the cause of meningitis may be the skin signs of hand, foot and mouth disease and genital herpes, both of which are associated with various forms of viral meningitis.[17]
Additional problems may occur in the early stage of the illness. These may require specific treatment, and sometimes indicate severe illness or worse prognosis. The infection may trigger sepsis, a systemic inflammatory response syndrome of falling blood pressure, fast heart rate, high or abnormally low temperature, and rapid breathing. Very low blood pressure may occur at an early stage, especially but not exclusively in meningococcal meningitis; this may lead to insufficient blood supply to other organs.[1] Disseminated intravascular coagulation, the excessive activation of blood clotting, may obstruct blood flow to organs and paradoxically increase the bleeding risk. Gangrene of limbs can occur in meningococcal disease.[1] Severe meningococcal and pneumococcal infections may result in hemorrhaging of the adrenal glands, leading to Waterhouse-Friderichsen syndrome, which is often fatal.[18]
The brain tissue may swell, pressure inside the skull may increase and the swollen brain may herniate through the skull base. This may be noticed by a decreasinglevel of consciousness, loss of the pupillary light reflex, and abnormal posturing.[3] The inflammation of the brain tissue may also obstruct the normal flow of CSF around the brain (hydrocephalus).[3] Seizures may occur for various reasons; in children, seizures are common in the early stages of meningitis (in 30% of cases) and do not necessarily indicate an underlying cause.[5] Seizures may result from increased pressure and from areas of inflammation in the brain tissue.[3] Focal seizures(seizures that involve one limb or part of the body), persistent seizures, late-onset seizures and those that are difficult to control with medication indicate a poorer long-term outcome.[1]
Inflammation of the meninges may lead to abnormalities of the cranial nerves, a group of nerves arising from the brain stem that supply the head and neck area and which control, among other functions, eye movement, facial muscles, and hearing.[1][13] Visual symptoms and hearing loss may persist after an episode of meningitis.[1] Inflammation of the brain (encephalitis) or its blood vessels (cerebral vasculitis), as well as the formation of blood clots in the veins (cerebral venous thrombosis), may all lead to weakness, loss of sensation, or abnormal movement or function of the part of the body supplied by the affected area of the brain.[1][3]
Meningitis is typically caused by an infection with microorganisms. Most infections are due to viruses,[13] with bacteria, fungi, and protozoa being the next most common causes.[4] It may also result from various non-infectious causes.[4] The term aseptic meningitis refers to cases of meningitis in which no bacterial infection can be demonstrated. This type of meningitis is usually caused by viruses but it may be due to bacterial infection that has already been partially treated, when bacteria disappear from the meninges, or pathogens infect a space adjacent to the meninges (e.g. sinusitis). Endocarditis (an infection of the heart valves which spreads small clusters of bacteria through the bloodstream) may cause aseptic meningitis. Aseptic meningitis may also result from infection with spirochetes, a type of bacteria that includes Treponema pallidum (the cause of syphilis) and Borrelia burgdorferi (known for causing Lyme disease). Meningitis may be encountered in cerebral malaria (malaria infecting the brain) or amoebic meningitis, meningitis due to infection with amoebae such as Naegleria fowleri, contracted from freshwater sources.[4]
Recent skull trauma potentially allows nasal cavity bacteria to enter the meningeal space. Similarly, devices in the brain and meninges, such as cerebral shunts, extraventricular drains or Ommaya reservoirs, carry an increased risk of meningitis. In these cases, the persons are more likely to be infected with Staphylococci, Pseudomonas, and other Gram-negative bacteria.[5] These pathogens are also associated with meningitis in people with an impaired immune system.[1] An infection in the head and neck area, such as otitis media or mastoiditis, can lead to meningitis in a small proportion of people.[5] Recipients of cochlear implants for hearing loss are more at risk for pneumococcal meningitis.[21]
Tuberculous meningitis, which is meningitis caused by Mycobacterium tuberculosis, is more common in people from countries in which tuberculosis is endemic, but is also encountered in persons with immune problems, such as AIDS.[22]
Recurrent bacterial meningitis may be caused by persisting anatomical defects, either congenital or acquired, or by disorders of the immune system.[23] Anatomical defects allow continuity between the external environment and the nervous system. The most common cause of recurrent meningitis is a skull fracture,[23] particularly fractures that affect the base of the skull or extend towards the sinusesand petrous pyramids.[23] Approximately 59% of recurrent meningitis cases are due to such anatomical abnormalities, 36% are due to immune deficiencies (such as complement deficiency, which predisposes especially to recurrent meningococcal meningitis), and 5% are due to ongoing infections in areas adjacent to the meninges.[23]
Viruses that cause meningitis include enteroviruses, herpes simplex virus (generally type 2, which produces most genital sores; less commonly type 1), varicella zoster virus (known for causingchickenpox and shingles), mumps virus, HIV, and LCMV.[17] Mollaret's meningitis is a chronic recurrent form of herpes meningitis; it is thought to be caused by herpes simplex virus type 2.[24]
There are a number of risk factors for fungal meningitis, including the use of immunosuppressants (such as after organ transplantation), HIV/AIDS,[25] and the loss of immunity associated with aging.[26] It is uncommon in those with a normal immune system[27] but has occurred with medication contamination.[28] Symptom onset is typically more gradual, with headaches and fever being present for at least a couple of weeks before diagnosis.[26] The most common fungal meningitis is cryptococcal meningitis due to Cryptococcus neoformans.[29] In Africa, cryptococcal meningitis is now the most common cause of meningitis in multiple studies,[30][31] and it accounts for 20–25% of AIDS-related deaths in Africa.[32] Other less common fungal pathogens which can cause meningitis include: Coccidioides immitis,Histoplasma capsulatum, Blastomyces dermatitidis, and Candida species.[26]
A parasitic cause is often assumed when there is a predominance of eosinophils (a type of white blood cell) in the CSF. The most common parasites implicated are Angiostrongylus cantonensis,Gnathostoma spinigerum, Schistosoma, as well as the conditions cysticercosis, toxocariasis, baylisascariasis, paragonimiasis, and a number of rarer infections and noninfective conditions.[33]
Meningitis may occur as the result of several non-infectious causes: spread of cancer to the meninges (malignant or neoplastic meningitis)[34] and certain drugs (mainly non-steroidal anti-inflammatory drugs, antibiotics and intravenous immunoglobulins).[35] It may also be caused by several inflammatory conditions, such as sarcoidosis (which is then called neurosarcoidosis), connective tissue disorders such as systemic lupus erythematosus, and certain forms of vasculitis (inflammatory conditions of the blood vessel wall), such as Behçet's disease.[4] Epidermoid cysts and dermoid cysts may cause meningitis by releasing irritant matter into the subarachnoid space.[4][23] Rarely, migraine may cause meningitis, but this diagnosis is usually only made when other causes have been eliminated.[4]
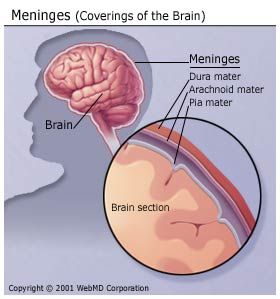
The meninges comprise three membranes that, together with the cerebrospinal fluid, enclose and protect the brain and spinal cord (the central nervous system). The pia mater is a very delicate impermeable membrane that firmly adheres to the surface of the brain, following all the minor contours. The arachnoid mater (so named because of its spider-web-like appearance) is a loosely fitting sac on top of the pia mater. The subarachnoid space separates the arachnoid and pia mater membranes and is filled with cerebrospinal fluid. The outermost membrane, the dura mater, is a thick durable membrane, which is attached to both the arachnoid membrane and the skull.
In bacterial meningitis, bacteria reach the meninges by one of two main routes: through the bloodstream or through direct contact between the meninges and either the nasal cavity or the skin. In most cases, meningitis follows invasion of the bloodstream by organisms that live upon mucous surfaces such as the nasal cavity. This is often in turn preceded by viral infections, which break down the normal barrier provided by the mucous surfaces. Once bacteria have entered the bloodstream, they enter the subarachnoid space in places where the blood–brain barrier is vulnerable—such as the choroid plexus. Meningitis occurs in 25% of newborns with bloodstream infections due to group B streptococci; this phenomenon is less common in adults.[1] Direct contamination of the cerebrospinal fluid may arise from indwelling devices, skull fractures, or infections of the nasopharynx or the nasal sinuses that have formed a tract with the subarachnoid space (see above); occasionally, congenital defects of the dura mater can be identified.[1]
The large-scale inflammation that occurs in the subarachnoid space during meningitis is not a direct result of bacterial infection but can rather largely be attributed to the response of the immune system to the entry of bacteria into the central nervous system. When components of the bacterial cell membrane are identified by the immune cells of the brain (astrocytes and microglia), they respond by releasing large amounts of cytokines, hormone-like mediators that recruit other immune cells and stimulate other tissues to participate in an immune response. The blood–brain barrier becomes more permeable, leading to "vasogenic" cerebral edema (swelling of the brain due to fluid leakage from blood vessels). Large numbers of white blood cells enter the CSF, causing inflammation of the meninges and leading to "interstitial" edema (swelling due to fluid between the cells). In addition, the walls of the blood vessels themselves become inflamed (cerebral vasculitis), which leads to decreased blood flow and a third type of edema, "cytotoxic" edema. The three forms of cerebral edema all lead to increased intracranial pressure; together with the lowered blood pressure often encountered in acute infection, this means that it is harder for blood to enter the brain, consequently brain cells are deprived of oxygen and undergo apoptosis (programmed cell death).[1]
It is recognized that administration of antibiotics may initially worsen the process outlined above, by increasing the amount of bacterial cell membrane products released through the destruction of bacteria. Particular treatments, such as the use of corticosteroids, are aimed at dampening the immune system's response to this phenomenon.[1][3]
| Type of meningitis | Glucose | Protein | Cells |
|---|---|---|---|
| Acute bacterial | low | high | PMNs, often > 300/mm³ |
| Acute viral | normal | normal or high | mononuclear, < 300/mm³ |
| Tuberculous | low | high | mononuclear and PMNs, < 300/mm³ |
| Fungal | low | high | < 300/mm³ |
| Malignant | low | high | usually mononuclear |
In someone suspected of having meningitis, blood tests are performed for markers of inflammation (e.g. C-reactive protein, complete blood count), as well as blood cultures.[5][37]
The most important test in identifying or ruling out meningitis is analysis of the cerebrospinal fluid through lumbar puncture (LP, spinal tap).[38]However, lumbar puncture is contraindicated if there is a mass in the brain (tumor or abscess) or the intracranial pressure (ICP) is elevated, as it may lead to brain herniation. If someone is at risk for either a mass or raised ICP (recent head injury, a known immune system problem, localizing neurological signs, or evidence on examination of a raised ICP), a CT or MRI scan is recommended prior to the lumbar puncture.[5][37][39] This applies in 45% of all adult cases.[3] If a CT or MRI is required before LP, or if LP proves difficult, professional guidelines suggest that antibiotics should be administered first to prevent delay in treatment,[5] especially if this may be longer than 30 minutes.[37][39]Often, CT or MRI scans are performed at a later stage to assess for complications of meningitis.[1]
In severe forms of meningitis, monitoring of blood electrolytes may be important; for example, hyponatremia is common in bacterial meningitis, due to a combination of factors, including dehydration, the inappropriate secretion of the antidiuretic hormone (SIADH), or overly aggressive intravenous fluid administration.[3][40]
A lumbar puncture is done by positioning the person, usually lying on the side, applying local anesthetic, and inserting a needle into the dural sac (a sac around the spinal cord) to collect cerebrospinal fluid (CSF). When this has been achieved, the "opening pressure" of the CSF is measured using a manometer. The pressure is normally between 6 and 18 cm water (cmH2O);[38] in bacterial meningitis the pressure is usually elevated.[5][37] In cryptococcal meningitis, intracranial pressure is markedly elevated.[41] The initial appearance of the fluid may prove an indication of the nature of the infection: cloudy CSF indicates higher levels of protein, white and red blood cells and/or bacteria, and therefore may suggest bacterial meningitis.[5]
The CSF sample is examined for presence and types of white blood cells, red blood cells, protein content and glucose level.[5] Gram staining of the sample may demonstrate bacteria in bacterial meningitis, but absence of bacteria does not exclude bacterial meningitis as they are only seen in 60% of cases; this figure is reduced by a further 20% if antibiotics were administered before the sample was taken. Gram staining is also less reliable in particular infections such as listeriosis.Microbiological culture of the sample is more sensitive (it identifies the organism in 70–85% of cases) but results can take up to 48 hours to become available.[5] The type of white blood cell predominantly present (see table) indicates whether meningitis is bacterial (usually neutrophil-predominant) or viral (usually lymphocyte-predominant),[5] although at the beginning of the disease this is not always a reliable indicator. Less commonly, eosinophils predominate, suggesting parasitic or fungal etiology, among others.[33]
The concentration of glucose in CSF is normally above 40% of that in blood. In bacterial meningitis it is typically lower; the CSF glucose level is therefore divided by the blood glucose (CSF glucose to serum glucose ratio). A ratio ?0.4 is indicative of bacterial meningitis;[38] in the newborn, glucose levels in CSF are normally higher, and a ratio below 0.6 (60%) is therefore considered abnormal.[5] High levels of lactate in CSF indicate a higher likelihood of bacterial meningitis, as does a higher white blood cell count.[38] If lactate levels are less than 35 mg/dl and the person has not previously received antibiotics then this may rule out bacterial meningitis.[42]
Various other specialized tests may be used to distinguish between different types of meningitis. A latex agglutination test may be positive in meningitis caused by Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae, Escherichia coli and group B streptococci; its routine use is not encouraged as it rarely leads to changes in treatment, but it may be used if other tests are not diagnostic. Similarly, the limulus lysate test may be positive in meningitis caused by Gram-negative bacteria, but it is of limited use unless other tests have been unhelpful.[5] Polymerase chain reaction(PCR) is a technique used to amplify small traces of bacterial DNA in order to detect the presence of bacterial or viral DNA in cerebrospinal fluid; it is a highly sensitive and specific test since only trace amounts of the infecting agent's DNA is required. It may identify bacteria in bacterial meningitis and may assist in distinguishing the various causes of viral meningitis (enterovirus, herpes simplex virus 2and mumps in those not vaccinated for this).[17] Serology (identification of antibodies to viruses) may be useful in viral meningitis.[17] If tuberculous meningitis is suspected, the sample is processed forZiehl-Neelsen stain, which has a low sensitivity, and tuberculosis culture, which takes a long time to process; PCR is being used increasingly.[22] Diagnosis of cryptococcal meningitis can be made at low cost using an India ink stain of the CSF; however, testing for cryptococcal antigen in blood or CSF is more sensitive, particularly in people with AIDS.[43][44]
A diagnostic and therapeutic difficulty is "partially treated meningitis", where there are meningitis symptoms after receiving antibiotics (such as for presumptive sinusitis). When this happens, CSF findings may resemble those of viral meningitis, but antibiotic treatment may need to be continued until there is definitive positive evidence of a viral cause (e.g. a positive enterovirus PCR).[17]
Meningitis can be diagnosed after death has occurred. The findings from a post mortem are usually a widespread inflammation of the pia mater and arachnoid layers of the meninges. Neutrophil granulocytes tend to have migrated to the cerebrospinal fluid and the base of the brain, along with cranial nerves and the spinal cord, may be surrounded with pus — as may the meningeal vessels.[45]