A cataract is a clouding of the lens inside the eye which leads to a decrease in vision. It is the most common cause of blindness and is conventionally treated with surgery. Visual loss occurs because opacification of the lens obstructs light from passing and being focused on the retina at the back of the eye.
Cataracts, a leading cause of blindness among adults 45 years of age and older, are a clouding of the eye's lens. Because of this cloudiness, light rays do not easily pass through the lens to focus on the retina. As a result, things look foggy or cloudy.
Most cataracts can be diagnosed with an eye exam. Your eye doctor will test your vision and examine your eyes with a slit lamp microscope to look for problems with the lens and other parts of the eye. The pupils are dilated to better examine the back of the eye, where the retina and optic nerve lie.
A nuclear cataract is the most common type of cataract, beginning with a gradual hardening and yellowing of the central zone of the lens, also known as the nucleus. Over time, this hardening and yellowing will expand to the other layers of the lens.
Cataracts are cloudy areas in the lens of the eye that can cause changes in vision. Symptoms of cataracts include cloudy or fuzzy vision as well as sensitivity to glare. Cataracts are treated with surgery.
What Are Cataracts?
Cataract is a clouding of the eye's lens. When we look at something, light rays travel into our eye through the pupil and are focused through the lens onto the retina, a layer of light-sensitive cells at the back of the eye. The lens must be clear in order to focus light properly onto the retina. If the lens has become cloudy, this is called a cataract.
Vision problems with cataracts
If your vision has become blurry, cloudy or dim, or things you see are not as bright or colorful as they used to be, a cataract may have developed in one or both of your eyes. Many people say that their vision with cataracts is similar to the effect of looking through a dirty car windshield.
Cataracts
are most commonly due to aging, but may also occur due to trauma, radiation exposure, be present from birth,
or occur following eye surgery for other problems.[1][6] Risk factors include diabetes, smoking tobacco, prolonged exposure
to sunlight, and alcohol. Either clumps of protein or yellow-brown pigment may be deposited in
the lens reducing the transmission of light to the retina at the back of the eye. Diagnosis is by an eye examination.[1]
Prevention
includes wearing sunglasses and not smoking. Early on the symptoms may
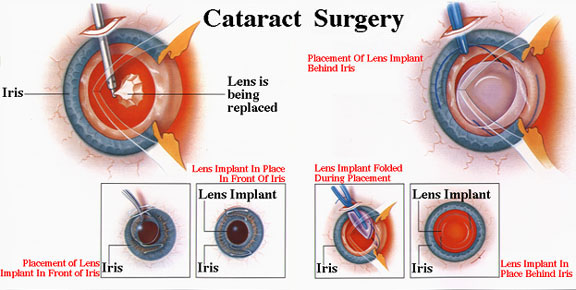
be improved with eyeglasses. If this does not help, surgery to remove the cloudy lens and replace it with an
artificial lens is the
only effective treatment. Surgery is only needed if the cataracts are causing
problems.[1] Surgery generally results in an improved quality of life.[7] Cataract surgery is not easily available in
many countries, which is especially true for women, those living in rural
areas, and those who cannot read.[6][8]
Signs and symptoms vary depending on the type of cataract, though
considerable overlap occurs. People with nuclear sclerotic or brunescent
cataracts often notice a reduction of vision. Those with posterior
subcapsular cataracts usually complain of glareas their major symptom.[10]
The severity of cataract formation, assuming no other
eye disease is present, is judged primarily by a visual acuity test. The
appropriateness of surgery depends on a patient's particular functional and
visual needs and other risk factors, all of which may vary widely.[11]
Causes
Age
Age is the most common cause.[1][6] Lens proteins denature and degrade over
time, and this process is accelerated by diseases such as diabetes mellitus and hypertension. Environmental factors, including
toxins, radiation, and ultraviolet light, have cumulative effects,
which are worsened by the loss of protective and restorative mechanisms due to
alterations in gene expression and chemical processes within the eye.[12]
Trauma
Blunt trauma causes swelling, thickening, and
whitening of the lens fibers. While the swelling normally resolves with time,
the white color may remain. In severe blunt trauma, or injuries which penetrate
the eye, the capsule in which the lens sits can be damaged. This allows fluid
from other parts of the eye to rapidly enter the lens leading to swelling and
then whitening, obstructing light from reaching the retina at the back of the
eye. Cataracts may develop in 0.7 to 8.0% of cases following electrical injuries.[13]
Radiation
Ultraviolet light, specifically UVB, has been shown to
cause cataracts, and some evidence indicates sunglasses worn at an early age
can slow its development in later life.[14] Microwave radiation
has also been found to cause cataracts. The mechanism is unclear, but it may
include changes in heat-sensitive enzymes that normally protect cell proteins
in the lens. Another possible mechanism is direct damage to the lens from
pressure waves induced in the aqueous humor.
Cataracts have been associated with ionizing radiation
such as X-rays. The addition of damage to the DNA of the lens cells has been
considered.[15] Finally, electric and
heat injuries denature and whiten the lens as a result of direct protein
coagulation.[12] This same process
makes the clear albumin of an egg become white and opaque after cooking.
Cataracts of this type are often seen in glassblowersand
furnace workers. Lasers of
sufficient power output are known to damage the eyes and skin.
Genetics
The genetic component is strong in the development of
cataracts,[16] most commonly through
mechanisms that protect and maintain the lens. The presence of cataracts in
childhood or early life can occasionally be due to a particular syndrome.
Examples of chromosome
abnormalities associated
with cataracts include 1q21.1 deletion
syndrome, cri-du-chat syndrome, Down syndrome, Patau's syndrome, trisomy 18 (Edward's syndrome),
and Turner's syndrome,
and in the case of neurofibromatosis
type 2, juvenile
cataract on
one or both sides may be noted. Examples of single-gene disorderinclude Alport's syndrome, Conradi's syndrome, myotonic dystrophy,
and oculocerebrorenal
syndrome or
Lowe syndrome.
Skin
diseases
The skin and the lens have the same embryological
origin and so can be affected by similar diseases.[17] Those with atopic dermatitis and eczema occasionally
develop shield ulcers cataracts. Ichthyosisis an autosomal recessive disorder
associated with cuneiform cataracts and nuclear sclerosis. Basal-cell nevus and pemphigus have
similar associations.
Drug
use
Cigarette smoking has been shown to
double the rate of nuclear sclerotic cataracts and triple the rate of posterior
subcapsular cataracts.[18] Evidence is
conflicting over the effect of alcohol. Some surveys have shown a link, but
others which followed patients over longer terms have not.[19]
Medications
Some drugs, such as corticosteroids, can induce cataract
development.[20] People with schizophrenia often have risk
factors for lens opacities (such as diabetes, hypertension, and poor nutrition)
butantipsychotic medications are
unlikely to contribute to cataract formation.[21] Miotics[22] and triparanol may
increase the risk.[23]
Healthcare
caused
Nearly every person who undergoes a vitrectomy —
without ever having had cataract surgery — will experience progression of nuclear sclerosis at 6-months and
12-month after the operation.[24] This may be because
the native vitreous humor is significantly different to the solutions used to
replace the vitreous (vitreous
substitutes), such as BSS Plus.[25] This may also be
because the native vitreous humour contains ascorbic acid which helps
neutralize oxidative damage to the lens and because traditional vitreous
substitutes do not contain ascorbic acid.[26][27] As such, for phakic
patients requiring a vitrectomy it is becoming increasingly common for
ophthalmologists to offer the vitrectomy with a combined prophylactic cataract surgery procedure to
prophylactically prevent cataract formation.[28]
Other
diseases
Cross-sectional view, showing the position of
the human lens
Cataracts may be partial or complete, stationary or progressive,
or hard or soft. The main types of age-related cataracts are nuclear sclerosis,
cortical, and posterior subcapsular.
Nuclear sclerosis, the most common type of cataract, involves
the central or 'nuclear' part of the lens. Over time, this becomes hard or
'sclerotic' due to condensation of lens nucleus and deposition of brown pigment
within the lens. In advanced stages, it is called brunescent cataract. This
type of cataract can present with a shift to nearsightedness and causes
problems with distance vision, while reading is less affected.[29]
Cortical cataracts are due to the lens cortex (outer layer)
becoming opaque. They occur when changes in the fluid contained in the
periphery of the lens causes fissuring. When these cataracts are viewed through
an ophthalmoscope or other magnification
system, the appearance is similar to white spokes of a wheel. Symptoms often
include problems with glare and light scatter at night.[29]
Posterior subcapsular cataracts are cloudy at back of the lens
adjacent to the capsule (or bag) in which the lens sits. Because light becomes
more focused toward the back of the lens, they can cause disproportionate
symptoms for their size.
An immature cataract has some transparent protein, but with a
mature cataract, all the lens protein is opaque. In a hypermature or Morgagnian
cataract, the lens proteins have become liquid. Congenital cataract, which may
be detected in adulthood, has a different classification and includes lamellar,
polar, and sutural cataracts.[20][30]
Cataracts can be classified by using the lens opacities
classification system LOCS III. In this system, cataracts are classified based
on type as nuclear, cortical, or posterior. The cataracts are further
classified based on severity on a scale from 1 to 5. The LOCS III system is
highly reproducible.[31]
Cataract symptom progression
- Painless cloudy, blurry or dim vision
- More difficulty seeing at night or in low light
- Sensitivity to light and glare
- Seeing halos around lights
- Faded or yellowed colors
- The need for brighter light for reading and other activities
- Frequent changes in eyeglass or contact lens prescription
- Double vision within one eye
See a simulation of what vision with cataract looks like.
The only way to know for certain if you have cataracts is to have a dilated eye exam (where your pupil is widened with eye drops). Your ophthalmologist can detect early signs of cataract development by looking at your eye's lens.
Get a baseline exam at age 40 when early signs of disease and changes in vision may start to occur. Your ophthalmologist (Eye M.D.) will let you know how often you should return for follow-up exams. At any point, if you have symptoms or risks for eye disease, see your Eye M.D. Because your risk for cataracts and other eye diseases increases as you get older, starting at age 65 you should see your Eye M.D. every year. A complete eye examination will rule out any other condition that may be causing blurred vision or eye problems. Early detection and treatment of cataracts is critical to preserving sight.
What Causes Cataracts?
Cataracts happen when protein builds up in the lens of your eye, making it cloudy. This prevents light from passing clearly through the lens, causing some loss of vision. New lens cells form on the outside of the lens, and the older cells are compacted into the center of the lens, forming the cataract.
Types of cataracts include:
- Age-related cataracts. These cataracts form because of of aging.
- Congenital cataracts. Babies are sometimes born with cataracts as a result of an infection, injury, or poor development before they were born, or they may develop during childhood.
- Secondary cataracts. These develop as a result of other medical conditions, like diabetes, or exposure to toxic substances, certain drugs (such as corticosteroids or diuretics), ultraviolet light, orradiation.
- Traumatic cataracts. These form after an injury to the eye.
Other things that can raise your risk of getting cataracts include cigarette smoke, air pollution, and heavy drinking.
A cataract is a clouding of the eye's natural lens, which lies behind theiris and the pupil.
Cataracts are the most common cause of vision loss in people over age 40 and is the principal cause of blindness in the world. In fact, there are more cases of cataracts worldwide than there are ofglaucoma, macular degeneration and diabetic retinopathy combined, according to Prevent Blindness America (PBA).

Types of cataracts include:
- A subcapsular cataract occurs at the back of the lens. People with diabetes or those taking high doses of steroid medications have a greater risk of developing a subcapsular cataract.
- A nuclear cataract forms deep in the central zone (nucleus) of the lens. Nuclear cataracts usually are associated with aging.
- A cortical cataract is characterized by white, wedge-like opacities that start in the periphery of the lens and work their way to the center in a spoke-like fashion. This type of cataract occurs in the lens cortex, which is the part of the lens that surrounds the central nucleus.
Cataract Symptoms and Signs
A cataract starts out small and at first has little effect on your vision. You may notice that your vision is blurred a little, like looking through a cloudy piece of glass or viewing an impressionist painting.
A cataract may make light from the sun or a lamp seem too bright or glaring. Or you may notice when you drive at night that the oncoming headlights cause more glare than before. Colors may not appear as bright as they once did.
The type of cataract you have will affect exactly which symptoms you experience and how soon they will occur. When a nuclear cataract first develops, it can bring about a temporary improvement in your near vision, called "second sight."
Unfortunately, the improved vision is short-lived and will disappear as the cataract worsens. On the other hand, a subcapsular cataract may not produce any symptoms until it's well-developed.
If you think you have a cataract, see an eye doctor for an exam to find out for sure.
What Causes Cataracts?
The lens inside the eye works much like a camera lens, focusing light onto the retina for clear vision. It also adjusts the eye's focus, letting us see things clearly both up close and far away.
The lens is mostly made of water and protein. The protein is arranged in a precise way that keeps the lens clear and lets light pass through it.
But as we age, some of the protein may clump together and start to cloud a small area of the lens. This is a cataract, and over time, it may grow larger and cloud more of the lens, making it harder to see.
No one knows for sure why the eye's lens changes as we age, forming cataracts. But researchers worldwide have identified factors that may cause cataracts or are associated with cataract development. Besides advancing age, cataract risk factors include:
- Ultraviolet radiation from sunlight and other sources
- Diabetes
- Hypertension
- Obesity
- Smoking
- Prolonged use of corticosteroid medications
- Statin medicines used to reduce cholesterol
- Previous eye injury or inflammation
- Previous eye surgery
- Hormone replacement therapy
- Significant alcohol consumption
- High myopia
- Family history
One theory of cataract formation that's gaining favor is that many cataracts are caused by oxidative changes in the human lens. This is supported by nutrition studies that show fruits and vegetables high inantioxidants may help prevent certain types of cataracts (see below).