Medi Services
Arthritis is very common but is not well understood. Actually, “arthritis” is not a single disease; it is an informal way of referring to joint pain or joint disease. There are more than 100 different types of arthritis and related conditions. People of all ages, sexes and races can and do have arthritis, and it is the leading cause of disability in America. More than 50 million adults and 300,000 children have some type of arthritis. It is most common among women and occurs more frequently as people get older.
Common arthritis joint symptoms include swelling, pain, stiffness and decreased range of motion. Symptoms may come and go. They can be mild, moderate or severe. They may stay about the same for years, but may progress or get worse over time. Severe arthritis can result in chronic pain, inability to do daily activities and make it difficult to walk or climb stairs. Arthritis can cause permanent joint changes. These changes may be visible, such as knobby finger joints, but often the damage can only be seen on X-ray. Some types of arthritis also affect the heart, eyes, lungs, kidneys and skin as well as the joints.
There are different types of arthritis:
Osteoarthritis is the most common type of arthritis. When the cartilage – the slick, cushioning surface on the ends of bones – wears away, bone rubs against bone, causing pain, swelling and stiffness. Over time, joints can lose strength and pain may become chronic. Risk factors include excess weight, family history, age and previous injury (an anterior cruciate ligament, or ACL, tear, for example).
When the joint symptoms of osteoarthritis are mild or moderate, they can be managed by:
balancing activity with rest
using hot and cold therapies
regular physical activity
maintaining a healthy weight
strengthening the muscles around the joint for added support
using assistive devices
taking over-the-counter (OTC) pain relievers or anti-inflammatory medicines
avoiding excessive repetitive movements
If joint symptoms are severe, causing limited mobility and affecting quality of life, some of the above management strategies may be helpful, but joint replacement may be necessary.
Osteoarthritis can prevented by staying active, maintaining a healthy weight, and avoiding injury and repetitive movements.
A healthy immune system is protective. It generates internal inflammation to get rid of infection and prevent disease. But the immune system can go awry, mistakenly attacking the joints with uncontrolled inflammation, potentially causing joint erosion and may damage internal organs, eyes and other parts of the body. Rheumatoid arthritis and psoriatic arthritis are examples of inflammatory arthritis. Researchers believe that a combination of genetics and environmental factors can trigger autoimmunity. Smoking is an example of an environmental risk factor that can trigger rheumatoid arthritis in people with certain genes.
With autoimmune and inflammatory types of arthritis, early diagnosis and aggressive treatment is critical. Slowing disease activity can help minimize or even prevent permanent joint damage. Remission is the goal and may be achieved through the use of one or more medications known as disease-modifying antirheumatic drugs (DMARDs). The goal of treatment is to reduce pain, improve function, and prevent further joint damage.
A bacterium, virus or fungus can enter the joint and trigger inflammation. Examples of organisms that can infect joints are salmonella and shigella (food poisoning or contamination), chlamydia and gonorrhea (sexually transmitted diseases) and hepatitis C (a blood-to-blood infection, often through shared needles or transfusions). In many cases, timely treatment with antibiotics may clear the joint infection, but sometimes the arthritis becomes chronic.
Uric acid is formed as the body breaks down purines, a substance found in human cells and in many foods. Some people have high levels of uric acid because they naturally produce more than is needed or the body can’t get rid of the uric acid quickly enough. In some people the uric acid builds up and forms needle-like crystals in the joint, resulting in sudden spikes of extreme joint pain, or a gout attack. Gout can come and go in episodes or, if uric acid levels aren’t reduced, it can become chronic, causing ongoing pain and disability.
Diagnosing Arthritis
Arthritis diagnosis often begins with a primary care physician, who performs a physical exam and may do blood tests and imaging scans to help determine the type of arthritis. An arthritis specialist, or rheumatologist, should be involved if the diagnosis is uncertain or if the arthritis may be inflammatory. Rheumatologists typically manage ongoing treatment for inflammatory arthritis, gout and other complicated cases. Orthopaedic surgeons do joint surgery, including joint replacements. When the arthritis affects other body systems or parts, other specialists, such as ophthalmologists, dermatologists or dentists, may also be included in the health care team.
What Can Be Done About Arthritis?
There are many things that can be done to preserve joint function, mobility and quality of life. Learning about the disease and treatment options, making time for physical activity and maintaining a healthy weight are essential. Arthritis is a commonly misunderstood disease. 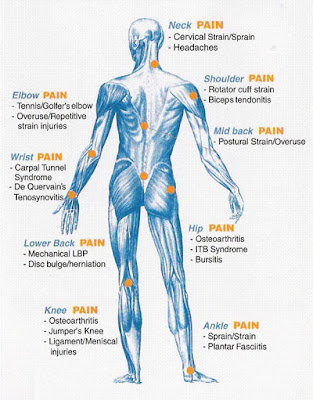
There is no single cause of all types of arthritis; the cause or causes in any given case vary according to the type or form of arthritis. Potential causes for arthritis may include:
Potential causes for arthritis may include:
Most types of arthritis are caused by a combination of many factors working together, although some arthritis conditions have no obvious cause and appear to be unpredictable in their emergence.
Some people may be more susceptible to certain arthritic conditions due to their genetic makeup. Additional factors, such as previous injury, infection, smoking and physically demanding occupations, can interact with a person's genes to further increase the risk of arthritis.

Diet and nutrition can play a role in managing arthritis and the risk of arthritis, although specific foods, food sensitivities or intolerances are not known to cause arthritis. Foods that increase inflammation, particularly animal-derived foods and diets high in refined sugar, can exacerbate arthritis. Similarly, eating foods that provoke an immune system response can exacerbate arthritis symptoms.
Gout is one type of arthritis that is closely linked to diet as it is caused by elevated levels of uric acid which can be a result of a diet high in purines. As such, diets that contain high-purine foods, such as seafood, red wine and meats can trigger a gout flare-up. Vegetables and other plant foods that contain high levels of purines do not appear to exacerbate gout symptoms, however.
Cartilage is a flexible, connective tissue in joints that absorb the pressure and shock created from movement like running and walking. It also protects the joints and allows for smooth movement.34
Rheumatoid arthritis occurs when the body's immune system attacks the tissues of the body, specifically connective tissue, leading to joint inflammation and pain and degeneration of the joint tissue.
There are around 200 types of arthritis - or musculoskeletal conditions - which are split into seven main groups:26
Inflammation is a normal part of the body's healing process. The inflammation tends to occur as a defense against viruses and bacteria or as a response to injuries such as burns. However, with inflammatory arthritis, inflammation occurs in people for no apparent reason.26

Inflammatory arthritis is characterized by damaging inflammation that does not occur as a normal reaction to injury or infection. This type of inflammation is unhelpful and instead causes damage in the affected joints, resulting in pain, stiffness and swelling.
The word "arthritis" means "joint inflammation," but inflammation may also affect the tendons and ligaments surrounding the joint - known as enthesitis.
Inflammatory arthritis can affect several joints, and the inflammation can damage the surface of the joints and also the underlying bone.
Examples of inflammatory arthritis include:
Degenerative or mechanical arthritis refers to a group of conditions primarily involving damage to the cartilage that covers the ends of the bones. The main job of the smooth, slippery cartilage is to help the joints glide and move smoothly. This type of arthritis causes the cartilage to become thinner and rougher.26
To compensate for the loss of cartilage and changes in joint function, the body begins to remodel the bone in an attempt to restore stability. This can cause undesirable bony growths to develop (osteophytes), or cause the joint to become misshapen. This condition is commonly called osteoarthritis.
Osteoarthritis can also result from previous damage to the joint such as a fracture or previous inflammation in the joint.
Soft tissue musculoskeletal pain is felt in tissues other than the joints and bones. The pain often affects a part of the body following injury or overuse, such as tennis elbow, and originates from the muscles or soft tissues supporting the joints.
Sometimes if the pain is more widespread and associated with other symptoms, it could be diagnosed as fibromyalgia.
Back pain can arise from the muscles, discs, nerves, ligaments, bones or joints. Back pain may even be caused by problems with organs inside the body, and can be a result of referred pain, i.e. a problem elsewhere in the body that causes a sensation of pain in the back.26
Back pain may have a specific cause, such as osteoarthritis - often called spondylosis when it occurs in the spine - which may be visible on diagnostic imaging or physical examination. A "slipped" disc is another cause of back pain, as is osteoporosis (thinning of the bones). In most cases it is not possible for a doctor to identify the exact cause of back pain - this is often described as "non-specific" pain.
Connective tissues are tissues that support, bind together or separate other body tissues and organs. They include tendons, ligaments and cartilage.26
Joint pain is a symptom of CTD, but the inflammation that characterizes CTD may also occur in other tissues including the skin, muscles, lungs and kidneys. This can result in a diverse range of symptoms besides painful joints and require consultation with a number of different specialists.
Examples of CTD include:
A bacterium, virus or fungus entering the joint can sometimes cause inflammation. Organisms that can infect joints include:27
In most of these cases, the joint infection can be cleared with antibiotics or other antimicrobial medication. However, the arthritis can sometimes become chronic, and/or joint damage may be irreversible if the infection has persisted for some time.
Uric acid is a chemical created when the body breaks down substances called purines. Purines are found in human cells and several foods.27
Most uric acid dissolves in blood and travels to the kidneys. From there, it passes out in urine. Some people have elevated levels of uric acid because they either naturally produce more than is needed or their body cannot clear the uric acid quickly enough.
Uric acid builds up and accumulates in some people and forms needle-like crystals in the joint, resulting in sudden spikes of extreme joint pain or a gout attack.
Gout can either come and go in episodes or become chronic if uric acid levels are not reduced. It commonly affects a single joint or a small number of joints, such as the big toe and hands, and usually affects the extremities. This is thought to be due in part to the increased formation of uric acid crystals in cooler joints, i.e. those not close to the main warmth of the body.
Some of the more common types of arthritis are discussed below.
There are an estimated 1.5 million adults in the US with RA.4 The prevalence of RA is believed to range from 0.5-1.0% in the general population.
Persistent inflammation in the synovia leads to the degeneration of cartilage and bone, which can then lead to joint deformity, pain, swelling and redness.
RA causes premature mortality, disability and compromises quality of life.12 The onset of RA can occur at any age and is associated with fatigue and prolonged stiffness after rest.
Individuals with RA have a more severe functional status than those with osteoarthritis. Diagnosing RA early gives people a better chance to learn how to manage symptoms successfully, which can reduce the impact of the disease on quality of life.
RA accounts for around 22% of all deaths due to AORC. Approximately 40% of all deaths in people with RA are attributed to cardiovascular conditions, including ischemic heart disease and stroke.
According to one review, the annual excess health care costs attributable to RA in the US in 2005 were $8.4 billion, and costs of other RA consequences were $10.9 billion. These costs translate to a total annual cost of $19.3 billion. A third (33%) of these costs are shouldered by employers, 28% by patients, 20% by the government, and 19% by caregivers. 54
This review also estimated that intangible costs of quality-of-life deterioration come to around $10.3 billion annually, and that premature mortality associated with rheumatoid arthritis costs the US $9.6 billion each year.54
For more information on rheumatoid arthritis, see our article: All about rheumatoid arthritis.

There are an estimated 26.9 million adults living with osteoarthritis in the US. Osteoarthritis affects 13.9% of adults aged 25 years and older, and 33.6% (12.4 million) of those over 65. Disease onset is gradual and often begins after the age of 40.55
Osteoarthritis is a degenerative joint disease of the entire joint involving the cartilage, joint lining and ligaments and underlying bone. The breakdown of these tissues eventually leads to pain and joint stiffness.11
The joints most commonly affected by osteoarthritis are the joints that get heavy use, such as hips and knees, hands, the spine and also often the base of the thumb and the big toe joint.
Nearly 1 in 2 people develop symptomatic knee osteoarthritis by the age of 85, and 1 in 4 people develop hip arthritis in their lifetime.4 Knee osteoarthritis is one of the five leading causes of disability among non-institutionalized adults. Weight loss of 11 pounds can halve a woman's risk of developing knee osteoarthritis.56
Taking part in moderate physical activity 3 times or more per week can reduce the risk of arthritis-related disability by 47% in older adults with knee osteoarthritis.4
The specific causes of osteoarthritis have not yet been identified but the condition is thought to be a result of mechanical and molecular events occurring in the affected joint.
Between 1979 and 1988, osteoarthritis was responsible for an average 0.2 to 0.3 deaths per 100,000 people. This figure has increased over the years, with OA accounting go around 6% of all arthritis-related deaths in 2003, working out to around 500 deaths per year.57
These calculations are likely to be underestimates as they do not include deaths related to things such as gastrointestinal bleeding caused by medications used to treat OA.
Costs due to hospital expenditures are estimated at $28.5 billion for knee replacements and $13.7 billion for hip replacements annually (2009).58 The average direct costs of osteoarthritis per patient is around $2,600 per year.53
For more information on osteoarthritis, see our article: What is osteoarthritis? What causes osteoarthritis?
There are an estimated 294,000 children (or 1 in 250 children) under the age of 18 in the US that have been diagnosed with AORC.
"Childhood arthritis" is an umbrella term that covers a number of types of arthritis.
There are at least three clinical classification schemes of childhood arthritis including:
All classifications define childhood arthritis as occurring in people younger than 16 years.
The most common form of childhood arthritis is JRA. JRA involves at least 6 weeks of incessant arthritis in children younger than 16 years with no other type of noticeable childhood arthritis.
Many of the numerous conditions that are counted as AORC in adults can also occur in children, although much more rarely.
During 2008-2010, physician visits for juvenile arthritis averaged more than1 million per year, and there were around 282,500 outpatient clinic visits for juvenile arthritis.59
Pediatric arthritis and other rheumatological conditions have a substantial economic impact, accounting for total hospital charges of $4.45 billion in 2012.59
There are an estimated 20,000 cases of septic arthritis in the US per year.37 The incidence of septic arthritis is around 2-10 cases per 100,000 in the general population and as high as 30-70 cases per 100,000 in patients with RA.38
Septic arthritis is joint inflammation due to a bacterial or fungal infection. If the septic arthritis is due to the bacteria that cause gonorrhea, it is described as gonococcal arthritis.23 The incidence of arthritis due to gonococcal infection is 2.8 cases per 100,000 person-years.
Joints commonly affected with septic arthritis include the knee and hip. Septic arthritis develops either when bacteria or other tiny disease-causing organisms (microorganisms) spread through the blood to a joint or when the joint is directly infected with a microorganism through injury or surgery.
Bacteria such as Staphylococcus or Streptococcus cause most cases of acute septic arthritis. Organisms such as Mycobacterium tuberculosis and Candida albicans cause chronic septic arthritis - which is less common than acute septic arthritis.
Septic arthritis may occur at any age. In children, it arises most often in those younger than 3 years. The hip is often the site of infection in infants.
Septic arthritis is uncommon from age 3 to adolescence. Children with septic arthritis are more likely than adults to be infected with Group B Streptococcus or Haemophilus influenzae if they have not been vaccinated. The incidence of bacterial arthritis caused by infection with H. influenzae has decreased almost 70% to 80% since the widespread use of H. influenzae b vaccine.38
The following conditions increase the risk of developing septic arthritis:
Septic arthritis is a rheumatologic emergency as joint destruction occurs rapidly and can lead to significant morbidity and mortality.37 Septic arthritis in RA is associated with a higher mortality rate of 25-30% due to delays in diagnosis and initiation of treatment.38
Fibromyalgia affects an estimated 5.0 million adults in the US.4 The prevalence of fibromyalgia is around 2%, with prevalence significantly higher among women (3.4%) than men (0.5%). Children can also have the disorder.
In 25-65% of cases, fibromyalgia co-occurs with other rheumatic conditions such as RA, SLE and ankylosing spondylitis.9
Individuals are usually diagnosed with fibromyalgia during middle age and prevalence increases with age.
Fibromyalgia is a disorder of unknown cause characterized by widespread pain, abnormal pain processing, sleep disturbance, fatigue and often, psychological distress.8
People that suffer from fibromyalgia have abnormal pain perception processing and react strongly to things that other people would not find painful.
Causes and risk factors of fibromyalgia are unknown. However there are some factors that have been loosely associated with disease onset such as:
Direct medical costs for fibromyalgia range between $3400-$3600 per person, per year. Total direct and indirect costs per person are $5,945.
Mortality among adults with fibromyalgia is similar to that of the general population. However, death rates from suicide and injuries are higher among fibromyalgia patients.8
For more information on fibromyalgia, see our article: What is fibromyalgia? What causes fibromyalgia?
Estimates of the prevalence of psoriatic arthritis in the US population vary between 0.3-1%, with a reported prevalence of 7-42% in patients with psoriasis.40
Psoriatic arthritis is a joint problem that often occurs with a skin condition called psoriasis.18
While most people with psoriatic arthritis develop psoriasis first and are later diagnosed with psoriatic arthritis, joint problems can occasionally occur prior to the emergence of psoriasis skin lesions.
Psoriatic arthritis occurs when the immune system attacks healthy cells and tissue. The abnormal immune response causes inflammation in the joints and an overproduction of skin cells.31
Several factors can increase the risk of psoriatic arthritis, including:32
The severity of psoriatic arthritis is reflected not only in the accrual of joint damage but also in increased mortality. Patients with psoriatic arthritis are at an increased risk for death with a standardized mortality ratio of 1.62 (meaning that 62% more deaths occur in people with the condition than in the general population).
The causes of death are similar to those in the general population, with cardiovascular causes being the most common.40 People with psoriatic arthritis tend to have a higher number of risk factors for cardiovascular disease than the general population, including increased BMI, triglycerides and C-reactive protein.60
There are around 8.3 million individuals that suffer from gout each year in the US; 6.1 million of whom are men and 2.2 million women.10 The incidence of gout among black men is almost twice that among white men.
Gout is a rheumatic disease that occurs due to the formation of uric acid crystals (monosodium urate) in tissues and fluids within the body. This process occurs because of an overproduction or under excretion of uric acid from the body.
Acute gout will typically manifest itself as a severely red, hot and swollen joint with agonizing pain. Gout may go into remission for long periods, followed by flares for days to weeks, or can become chronic. Recurrent attacks of acute gout can lead to a degenerative form of chronic arthritis called gouty arthritis.

Contributory risk factors for gout include:

Most cases of arthritis are diagnosed with a detailed medical history of current and past symptoms, physical examination and particular radiographic and laboratory studies. It is possible to have more than one form of arthritis at the same time, and only a few rheumatic diseases have a definitive diagnosis, such as gout.9
The tests ordered during the diagnostic process will depend on the type of arthritis suspected. Some tests that may be completed to make a diagnosis are:15,16,17,19,22

With osteoarthritis, a physical exam can show:16
RA is diagnosed clinically, but classified according to the 2010 American College of Rheumatology (ACR) and European League Against Rheumatism (EULAR) classification criteria for rheumatoid arthritis.12
Diagnosis of SLE can be very difficult. The gold standard is a rheumatologist's diagnosis. The American College of Rheumatology (ACR) uses a standard classification scheme requiring 4 of 11 criteria for research definition, although this is recognized to miss early and mild cases.
There are several diseases where joint pain is primary, and is considered the main feature. Generally when a person has "arthritis" it means that they have one of these diseases, which include:
Joint pain can also be a symptom of other diseases. In this case, the arthritis is considered to be secondary to the main disease; these include:
An undifferentiated arthritis is an arthritis that does not fit into well-known clinical disease categories, possibly being an early stage of a definite rheumatic disease.[9]
Disability due to musculoskeletal disorders increased by 45% from 1990 to 2010. Of these, osteoarthritis is the fastest increasing major health condition.[10] Among the many reports on the increased prevalence of musculoskeletal conditions, data from Africa are lacking and underestimated. A systematic review assessed the prevalence of arthritis and included twenty population-based and seven hospital-based studies.[11] The majority of studies, twelve, were from South Africa. Nine studies were well-conducted, eleven studies were of moderate quality, and seven studies were conducted poorly. The results of the systematic review were as follows:
| Extra-articular features of joint disease[12] |
|---|
| Cutaneous nodules |
| Cutaneous vasculitis lesions |
| Lymphadenopathy |
| Oedema |
| Ocular inflammation |
| Urethritis |
| Tenosynovitis (tendon sheath effusions) |
| Bursitis (swollen bursa) |
| Diarrhea |
| Orogenital ulceration |
Pain, which can vary in severity, is a common symptom in virtually all types of arthritis. Other symptoms include swelling, joint stiffness and aching around the joint(s). Arthritic disorders like lupus and rheumatoid arthritis can affect other organs in the body, leading to a variety of symptoms.[13] Symptoms may include:
It is common in advanced arthritis for significant secondary changes to occur. For example, arthritic symptoms might make it difficult for a person to move around and/or exercise, which can lead to secondary effects, such as:
These changes, in addition to the primary symptoms, can have a huge impact on quality of life.
Arthritis is the most common cause of disability in the USA. More than 20 million individuals with arthritis have severe limitations in function on a daily basis.[14] Absenteeism and frequent visits to thephysician are common in individuals who have arthritis. Arthritis can make it very difficult for individuals to be physically active and some become home bound.
It is estimated that the total cost of arthritis cases is close to $100 billion of which almost 50% is from lost earnings. Each year, arthritis results in nearly 1 million hospitalizations and close to 45 million outpatient visits to health care centers.[15]
Decreased mobility, in combination with the above symptoms, can make it difficult for an individual to remain physically active, contributing to an increased risk of obesity, high cholesterol or vulnerability to heart disease.[16] People with arthritis are also at increased risk of depression, which may be a response to numerous factors, including fear of worsening symptoms.[17]
Diagnosis is made by clinical examination from an appropriate health professional, and may be supported by other tests such as radiology and blood tests, depending on the type of suspected arthritis.[18]All arthritides potentially feature pain. Pain patterns may differ depending on the arthritides and the location. Rheumatoid arthritis is generally worse in the morning and associated with stiffness; in the early stages, patients often have no symptoms after a morning shower. Osteoarthritis, on the other hand, tends to be worse after exercise. In the aged and children, pain might not be the main presenting feature; the aged patient simply moves less, the infantile patient refuses to use the affected limb.[citation needed]
Elements of the history of the disorder guide diagnosis. Important features are speed and time of onset, pattern of joint involvement, symmetry of symptoms, early morning stiffness, tenderness, gelling or locking with inactivity, aggravating and relieving factors, and other systemic symptoms. Physical examination may confirm the diagnosis, or may indicate systemic disease. Radiographs are often used to follow progression or help assess severity.
Blood tests and X-rays of the affected joints often are performed to make the diagnosis. Screening blood tests are indicated if certain arthritides are suspected. These might include: rheumatoid factor,antinuclear factor (ANF), extractable nuclear antigen, and specific antibodies.
Treatment with DMARDs is designed to initiate an adaptive immune response, in part by CD4+ T helper (Th) cells, specifically Th17 cells.[21] Th17 cells are present in higher quantities at the site of bone destruction in joints and produce inflammatory cytokines associated with inflammation, such as interleukin-17 (IL-17).[22]
Bone erosion is a central feature of rheumatoid arthritis. Bone continuously undergoes remodeling by actions of bone resorbing osteoclasts and bone forming osteoblasts. One of the main triggers of bone erosion in the joints in rheumatoid arthritis is inflammation of the synovium, caused in part by the production of pro-inflammatory cytokines and receptor activator of nuclear factor kappa B ligand (RANKL), a cell surface protein present in Th17 cells and osteoblasts.[22] Osteoclast activity can be directly induced by osteoblasts through the RANK/RANKL mechanism.[23]

| Osteoarthritis | Rheumatoid arthritis | Gouty arthritis | |
|---|---|---|---|
| Speed of onset | Months | Weeks-months[28] | Hours for an attack[29] |
| Main locations | Weight-bearing joints (such as knees, hips, vertebral column) and hands | Hands (proximal interphalangeal and metacarpophalangeal joint) wrists, ankles, kneesand hips | Great toe, ankles, knees andelbows |
| Inflammation | May occur, though often mild compared to inflammation in rheumatoid arthritis | Yes | Yes |
| Radiologicchanges |
|
|
|
| Laboratory findings | None | Anemia, elevated ESR and C-reactive protein (CRP), rheumatoid factor, anti-citrullinated protein antibody | Crystal in joints |
| Other features |
|
|
Infectious arthritis is another severe form of arthritis. It presents with sudden onset of chills, fever and joint pain. The condition is caused by bacteria elsewhere in the body. Infectious arthritis must be rapidly diagnosed and treated promptly to prevent irreversible joint damage.[30]
Psoriasis can develop into psoriatic arthritis. With psoriatic arthritis, most individuals develop the skin problem first and then the arthritis. The typical features are of continuous joint pains, stiffness and swelling. The disease does recur with periods of remission but there is no cure for the disorder. A small percentage develop a severe painful and destructive form of arthritis which destroys the small joints in the hands and can lead to permanent disability and loss of hand function.[31]
