Medi Services

An ear infection (acute otitis media) is most often a bacterial or viral infection that affects the middle ear, the air-filled space behind the eardrum that contains the tiny vibrating bones of the ear. Children are more likely than adults to get ear infections.
Ear infections frequently are painful because of inflammation and buildup of fluids in the middle ear.
Because ear infections often clear up on their own, treatment may begin with managing pain and monitoring the problem. Ear infection in infants and severe cases in general often require antibiotic medications. Long-term problems related to ear infections — persistent fluids in the middle ear, persistent infections or frequent infections — can cause hearing problems and other serious complications.
The onset of signs and symptoms of ear infection is usually rapid.
Signs and symptoms common in children include:
Common signs and symptoms in adults include:
Signs and symptoms of an ear infection can indicate a number of conditions. It's important to get an accurate diagnosis and prompt treatment. Call your child's doctor if:
An adult with ear pain or discharge should see a doctor as soon as possible.
An ear infection is caused by a bacterium or virus in the middle ear. This infection often results from another illness — cold, flu or allergy — that causes congestion and swelling of the nasal passages, throat and eustachian tubes.
The eustachian tubes are a pair of narrow tubes that run from each middle ear to high in the back of the throat, behind the nasal passages. The throat end of the tubes open and close to:
Swelling, inflammation and mucus in the eustachian tubes from an upper respiratory infection or allergy can block them, causing the accumulation of fluids in the middle ear. A bacterial or viral infection of this fluid is usually what produces the symptoms of an ear infection.
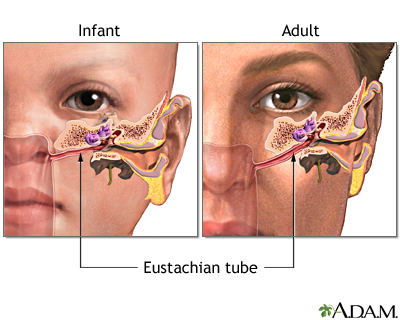
Ear infections are more common in children, in part, because their eustachian tubes are narrower and more horizontal — factors that make them more difficult to drain and more likely to get clogged.
Adenoids are two small pads of tissues high in the back of the nose believed to play a role in immune system activity. This function may make them particularly vulnerable to infection, inflammation and swelling.
Because adenoids are near the opening of the eustachian tubes, inflammation or enlargement of the adenoids may block the tubes, thereby contributing to middle ear infection. Inflammation of adenoids is more likely to play a role in ear infections in children because children have relatively larger adenoids.
Conditions of the middle ear that may be related to an ear infection or result in similar middle ear problems include the following:
Risk factors for ear infections include:
Most ear infections don't cause long-term complications. Frequent or persistent infections and persistent fluid buildup can result in some serious complications:
An instrument called a pneumatic otoscope is often the only specialized tool a doctor needs to make a diagnosis of an ear infection. This instrument enables the doctor to look in the ear and judge whether there is fluid behind the eardrum. With the pneumatic otoscope, the doctor gently puffs air against the eardrum. Normally, this puff of air would cause the eardrum to move. If the middle ear is filled with fluid, your doctor will observe little to no movement of the eardrum.
Your doctor may perform other diagnostic tests if there is any doubt about a diagnosis, if the condition hasn't responded to previous treatments, or if there are other persistent or serious problems.
Middle ear infections are caused by bacteria and viruses.
Swelling from an upper respiratory infection or allergy can block theeustachian tubes, which connect the middle ears to the throat. So air can't reach the middle ear. This creates a vacuum and suction, which pulls fluid and germs from the nose and throat into the middle ear. The swollen tube prevents this fluid from draining. The fluid is a perfect breeding ground for bacteria or viruses to grow into an ear infection.
Inflammation and fluid buildup can occur without infection and cause a feeling of stuffiness in the ears. This is known as otitis media with effusion.
Symptoms of a middle ear infection (acute otitis media) often start 2 to 7 days after the start of a cold or other upper respiratory infection. Symptoms of an ear infection may include:
The Eustachian tube runs from the middle of each ear to the back of the throat. This tube drains fluid made in the middle ear. If the Eustachian tube becomes blocked, fluid can build up. When this happens, infection can occur. A chronic ear infection develops when fluid or an infection behind the eardrum does not go away.

A chronic ear infection may be caused by:
"Suppurative chronic otitis" is a phrase health care providers use to describe an eardrum that keeps rupturing, draining, or swelling in the middle ear or mastoid area and does not go away.
Ear infections are more common in children because their Eustachian tubes are shorter, narrower, and more horizontal than in adults. Chronic ear infections are much less common than acute ear infections.
Symptoms of a chronic ear infection may be less severe than symptoms of an acute infection. The problem may go unnoticed and untreated for a long time.
Symptoms may include:
Symptoms may continue or come and go. They may occur in one or both ears.
The health care provider will examine the ears. This may reveal:
Tests may include:
Ear infections can be chronic or acute. Acute ear infections are painful but short in duration. Chronic ear infections do not clear up, or they recur many times. Chronic ear infections can cause permanent damage to the middle and inner ear
.