Medi Services

Keratitis

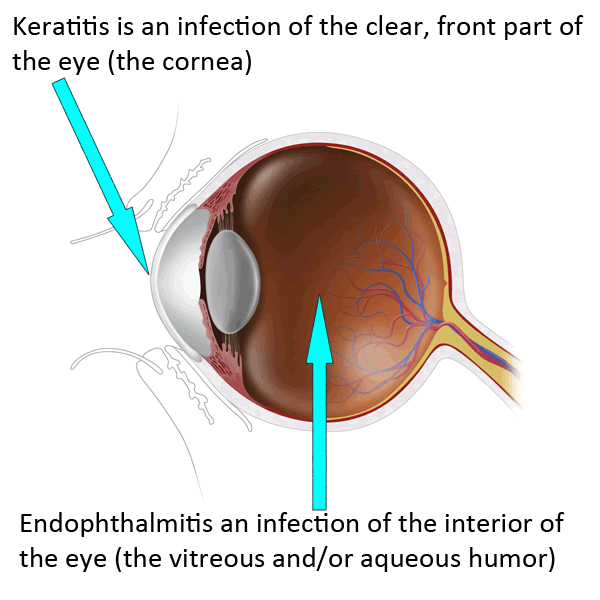
Keratitis is an inflammation of the cornea — the clear, dome-shaped tissue on the front of your eye that covers the pupil and iris. Keratitis is sometimes caused by an infection involving bacteria, viruses, fungi or parasites. Noninfectious keratitis can be caused by a minor injury, wearing your contact lenses too long or other noninfectious diseases.
If you have eye redness or other symptoms of keratitis, make an appointment to see your doctor. With prompt attention, mild to moderate cases of keratitis can usually be effectively treated without loss of vision. If left untreated, or if an infection is severe, keratitis can lead to serious complications that may permanently damage your vision.
Signs and symptoms of keratitis include:
If you notice any of the signs or symptoms of keratitis, make an appointment to see your doctor right away. Delays in diagnosis and treatment of keratitis can lead to serious complications, including vision loss.
Keratitis facts
Keratitis is the
medical term for inflammation of the cornea. The cornea is the dome-shaped
window in the front of the eye. When looking at a person's eye, one can see the iris and pupil
through the normally clear cornea. The cornea bends light rays as a result of
its curved shape and accounts for approximately two-thirds of the eye's total
optical power, with thelens of the eye contributing the
remaining one-third. Only the very thin tear film lies between the front of the
cornea and our environment.
The cornea is about
0.5 millimeter thick. The back of the cornea is bathed in the aqueous fluid
that fills the anterior chamber of the eye. The cornea has a diameter of about
13 millimeters (½ inch) and, together with the sclera (the white part of the
eye) forms the entire outer coat of the eye.
What are the causes of keratitis?
Keratitis, the eye
condition in which the cornea becomes inflamed, has many potential causes.
Various types of infections, dry eyes, injury, and a
large variety of underlying medical diseases may all lead to keratitis. Some
cases of keratitis result from unknown factors.
What are the different types of keratitis?
·
·
Keratitis can be
classified by its location, severity, and cause.
If keratitis only
involves the surface (epithelial) layer of the cornea, it is called superficial
keratitis. If it affects the deeper layers of the cornea (the corneal stroma),
it is called stromal keratitis or interstitial keratitis . It may involve the
center of the cornea or the peripheral part of the cornea (that portion closest
to the sclera) or both. Keratitis may affect one eye or both eyes.
Keratitis may be mild,
moderate, or severe and may be associated with inflammation of other parts of
the eye. Keratoconjunctivitis is inflammation of the cornea and the conjunctiva. Kerato-uveitis is
inflammation of the cornea and the uveal tract, which consists of the iris,
ciliary body, and choroid.
Keratitis may be acute
or chronic. It may occur only once or twice in an eye or be recurrent. It may
be limited in its effects on the eye or be progressive in its damage.
The various causes of
keratitis may result in different clinical presentations, so defining the
location, severity, and frequency of the condition can often assist in pinpointing
the exact cause. Other helpful facts in establishing the cause of keratitis can
include demographic information such as the age, sex, and geographic location
of the patient. A medical history is often useful as well in finding the cause
of keratitis.
Infection is the most
frequent cause of keratitis. Bacteria, viruses, fungi, and
parasitic organisms may all infect the cornea, causing infectious or microbial
keratitis.
Physical or chemical trauma is a frequent cause of
keratitis. The injury may become secondarily infected or remain noninfectious.
Retained corneal foreign bodies are frequent sources of keratitis. Ultraviolet
light from sunlight (snow blindness), a tanning light or a welder's arc,
contact-lens overwear, and chemical agents, either in liquid form splashed into
the eye or in gases in the form of fumes can all result in noninfectious
keratitis. Chemical injury or contact lens-related keratitis often causes
superficial punctate keratitis, in which the examiner notices myriads of
injured surface cells on the affected cornea.
Disturbances in the
tear film may lead to changes in the corneal surface through drying of the
corneal epithelium. This type of keratitis is usually superficial and is known
as keratitis sicca. If the eyes are extremely dry, the surface cells may die
and form attached filaments on the corneal surface, a condition known as
filamentary keratitis. Inability to close the eyelids properly can also lead to
corneal drying, a condition termed exposure keratitis.
Major risk factors for
the development of keratitis include any break or disruption of the surface
layer (epithelium) of the cornea.
The use of contact lenses increases the risk of
developing keratitis, especially if hygiene is poor, improper solutions are
used to store and clean the lenses, or if contact lenses are worn improperly or
in the presence of persistent irritation.
A decrease in the
quality or quantity of tears predisposes the eye to the development of
keratitis.
Disturbances of immune
function through diseases such as AIDS or the use of medications such as corticosteroids or chemotherapy also increase the risk of
developing keratitis.
What are keratitis symptoms and signs?
The symptoms of
keratitis usually include pain,
tearing, redness, and blurring of vision. The pain may be
mild to severe, depending on the cause and extent of the inflammation.
Sensitivity to light may also be present. To the observer, the eye may appear
red and watery; and if the cornea has extensive keratitis, the normally clear
cornea may look gray or have white to gray areas.
The diagnosis of
keratitis is made by an ophthalmologist (a physician who specializes in
diseases and surgery of the eye) through a history and a physical examination.
The history consists of questions documenting a past medical and ocular history
and the symptoms specific to the current visit. The eye examination will
consist of checking your vision and careful inspection of the corneas using a
slit lamp, which is a microscope with excellent illumination and magnification
to view the ocular surface and the cornea in detail. Special dye in the form of
eyedrops may be placed in the eyes to assist with the examination.
In cases in which
infection is suspected, a culture may be taken from the surface of the eye for
specific identification of the bacteria, virus, fungus, or parasite causing the
keratitis. Blood tests may also be done in certain patients with suspected
underlying disease.

Treatment depends on the cause of the keratitis. Infectious keratitis generally requires antibacterial, antifungal, or antiviral therapy to treat the infection. This treatment can involve prescription eyedrops, pills, or even intravenous therapy. Any corneal or conjunctivalforeign body should be removed. Wetting drops may be used if disturbance of the tears is suspected to be the cause of the keratitis. Steroid drops may be prescribed occaisionally to reduce inflammation and limit scarring. This must be done carefully and judiciously, since some infections can be worsened with their use.
Copyright © 2016 Seeking . All Rights Reserved . Design by Bluecircle
