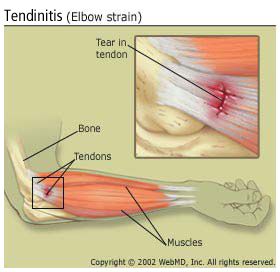
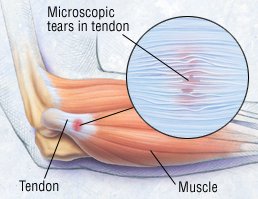
Loss of motion in the shoulder, called "adhesive capsulitis" or frozen shoulder.Tendons are tough, flexible, fibrous bands of tissue that connect muscles to bones. When tendons become inflamed, irritated or suffer microscopic tears, the condition is called tendonitis. Tendons can be small, like the delicate, tiny bands in the hands, or large, like the heavy, ropelike cords that anchor the calf or thigh muscles. In most cases, the cause of tendonitis is unknown; when a cause can be identified, the condition usually happens for one of two reasons:Overuse – A particular body motion is repeated too often.
Overload – The level of a certain activity, such as weightlifting, is increased too quickly.
Rarely, tendonitis is caused by an infection, such as gonorrhea. Tendonitis is most common in the shoulder, elbow, knee, wrist and heel, although it can happen anywhere that tendons are found in the body. For uncertain reasons, tendonitis is also common in people with diabetes. In recent years, a rare cause of tendonitis (or other tendon disease, including rupture) has been recognized: the use of certain antibiotics, including ciprofloxacin orlevofloxacin. Why this happens is unknown.
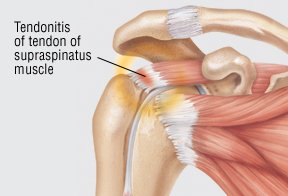
Tendonitis in the shoulder – The most common form of tendonitis in the shoulder is rotator cuff tendonitis. It involves the tendon of the supraspinatus muscle, which attaches to the upper portion of the upper arm bone (humerus) at the shoulder joint. Less commonly, the tendon of the infraspinatus muscle or other tendons of the rotator cuff is affected. In most cases, the supraspinatus tendon is injured by overuse, typically in an occupation or sport that requires the arm to be elevated repeatedly. People at risk include carpenters, painters, welders, swimmers, tennis players and baseball players. The average patient is a male laborer older than 40, and the shoulder pain is on the same side as his dominant hand (for example, right shoulder pain in a right-handed person).
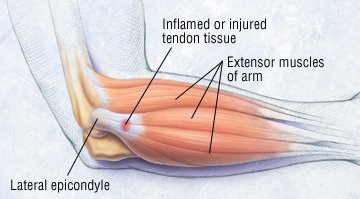
Tendonitis in the elbow – Two forms of tendonitis commonly involve the elbow: lateral epicondylitis and medial epicondylitis. Both are very common overuse injuries among athletes involved in throwing and racquet sports.
Lateral epicondylitis (tennis elbow) causes pain on the outer side of the elbow joint. This condition probably affects 40% to 50% of all adult athletes who play racquet sports. It also can be caused by any activity that repeatedly twists and flexes the wrist, such as pulling weeds, using a screwdriver or even carrying a briefcase.
Medial epicondylitis (golfer's elbow) causes pain on the inner side of the elbow. It is a less common injury than tennis elbow and, despite its name, it is more likely to be related an occupation that requires repeated elbow movements (such as construction work) than to sports. When it does occur as a sports injury, medial epicondylitis can be triggered by repeatedly swinging a golf club or throwing a baseball.
Tendonitis in the knee – Jumper's knee, the most common form of knee tendonitis, involves either the patellar tendon at the lower edge of the kneecap or the quadriceps tendon at the upper edge of the kneecap. It is a common overuse injury, especially in basketball players and distance runners.
Tendonitis in the wrist – In the wrist, tendonitis commonly appears in the form of de Quervain's disease, a condition that causes pain in the back of the wrist at the base of the thumb. Although de Quervain's disease usually occurs in people who repeatedly grasp or pinch with the thumb, it sometimes develops during pregnancy or for no known reason.
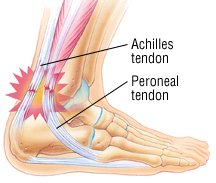
Achilles tendonitis – This form of tendonitis affects the Achilles tendon, the large ropelike tendon attached to the heel bone at the back of the foot. Achilles tendonitis usually is caused by overuse, especially in sports that require running or repeated jumping, and it accounts for 15% of all running injuries. Achilles tendonitis also may be related to faulty running technique or to poorly fitting shoes, if the back of the shoe digs into the Achilles tendon above the heel. Less often, Achilles tendonitis is related to an inflammatory illness, such as ankylosing spondylitis, reactive arthritis, gout or rheumatoid arthritis.
Symptoms
In general, tendonitis causes pain in the tissues surrounding a joint, especially after the joint is used too much during play or work. In some cases, the joint may feel weak, and the area may be red, swollen and warm to the touch.
When tendonitis is caused by an infection such as gonorrhea, there may be other symptoms, including rash, fever, or a discharge from the vagina or penis.
Other symptoms vary according to which tendon is affected:
Rotator cuff tendonitis – Usually dull, aching shoulder pain that can't be tied to one location. It often radiates into the upper arm toward the chest. The pain is often worse at night and may interfere with sleep.
Tennis elbow – Pain in the outer side of the elbow. In some cases, the painful area extends down to the forearm and wrist
Golfer's elbow – Pain in the inner side of the elbow
Jumper's knee – Pain below the kneecap and, sometimes, above it
De Quervain's disease – Pain at the back of the wrist, near the base of the thumb
Achilles tendonitis – Pain at the back of the heel or 2 to 4 inches above the heel
Diagnosis
After reviewing your medical history, including any previous joint injuries, your doctor will ask you specific questions about your pain:
What does your pain feel like (sharp, dull, burning)?
Where is your pain located? Is it limited to one area or does it spread away from the joint to involve a wider area on your arm, leg or hand?
Do you have tingling, numbness or weakness?
When did your pain start? Did it begin after a sudden increase in your work activities or exercise? Might it be related to any new sport or exercise that you've recently tried?
What makes it feel better, and what makes it worse?
Does the pain disappear when you rest the area, or is it present even at rest?
Have you had unprotected sex?
During the physical exam, your doctor will look for tenderness, swelling, redness, muscle weakness and limited motion in the area of the sore tendon. Your doctor also may ask you to move in certain ways, such as raising your arm above your head or bending your wrist. These moves may hurt, but they are very important to help your doctor figure out which tendon is affected. In most cases, the diagnosis can be made based on your medical history and symptoms, together with your occupational and sports history and the results of your physical examination.
Some people may need blood tests to look for other causes of inflammation around the joints, such as gout or rheumatoid arthritis. X-rays also may be taken to confirm that there is no fracture, dislocation or bone disease. In people with Achilles tendonitis or rotator cuff tendonitis, ultrasound or magnetic resonance imaging (MRI) scans may be used to help evaluate the extent of tendon damage.
Introduction
Tendons are strong bands or cords of tissue that attach muscle to bone. They help move the bones and joints when muscles contract.
The main types of tendon injury are:
- tendonitis – inflammation of a tendon
- tendinopathy – the gradual deterioration of a tendon
- tenosynovitis – inflammation of the protective sheath that surrounds a tendon
- tendon rupture – a sudden tear in a tendon
Tendon injuries usually happen during sports or activities that involve sudden, sharp movements, such as throwing or jumping, or after repeated overuse of the tendons, such as running.
They can also be caused by repetitive daily activities, such as regularly using a computer keyboard and mouse. This is known as a repetitive strain injury (RSI).
Symptoms of a tendon injury
Tendon injuries can affect many different parts of the body. Commonly affected areas include the shoulders, elbows, wrists, knees, fingers and backs of the heels.
Symptoms of a tendon injury can include:
- pain that gets worse when you move the affected area
- stiffness in the affected area, which may be worse in the morning
- weakness in the affected area or being unable to move a joint
- a sensation that the tendon is grating or crackling as it moves
- swelling, sometimes with heat or redness
- a lump on the affected tendon
If your tendon ruptures, you will usually experience sudden and severe pain, which may eventually settle into a continuous, dull ache or no pain at all. Movement in the affected area may also become more difficult or even impossible.
Read more about the symptoms of tendon injuries.
When to see your GP
Minor tendon injuries can often be treated at home (see below). They will usually get better in a few weeks.
See your GP if your symptoms are severe or don't start to improve within a few weeks, or if you think you may have ruptured a tendon.
Your GP will usually be able to diagnose a tendon injury by asking about your symptoms and examining the affected area. Occasionally, they may request an X-ray, ultrasound scan or magnetic resonance imaging (MRI) scan to confirm the diagnosis.
Some medications may be related to tendon injuries, such as fluoroquinolone antibiotics and statins, so your GP may stop these if you’re taking them.
Tendinitis, also known as tendonitis, is the inflammation of a tendon. Tendinitis is a type of tendinopathy - a disease of the tendon. Tendinosis is similar to tendinitis, but requires different treatment. Tendinitis refers to larger-scale acute (sudden, short-term) injuries with inflammation.
Usually tendinitis is referred to by the body part involved, for example, Achilles tendinitis which affects the Achilles tendon, or patellar tendinitis which affects the patellar tendon (jumper's knee). Tendinitis can occur in various other parts of the body, including the elbow, wrist, finger, or thigh. It is caused by overusing a tendon or injuring it, as may happen during sport.
Tendinitis can affect people of any age, but is more common among adults who do a lot of sports. Elderly individuals are also susceptible to tendinitis because our tendons tend to lose their elasticity and become weaker as we get older.
Some common lay terms for tendinitis include:
- Golfer's elbow
- Jumper's knee
- Pitcher's shoulder
- Swimmer's shoulder
- Tennis elbow
What are tendons?
A tendon is tissue which attaches muscle to bone. It is flexible, tough and fibrous and is capable of withstanding tension. A ligament extends from bone to bone at a joint, while a tendon extends from muscle to bone. Tendons and muscles work together and can only exert a pulling force. Although tendons and ligaments are tough and fibrous, they are referred to as soft tissue, because of their common comparison to bone or cartilage.
The Latin word tendere and the Greek word teinein mean "to stretch".
Inflamed tendons (tendinitis) are more likely to get ruptured. If the sheath around the tendon becomes inflamed, rather than the tendon itself, the condition is called tenosynovitis. People can have tendinitis and tenosynovitis simultaneously.
Symptoms of tendinitis
A symptom is something the patient feels and reports, while a sign is something other people, such as the doctor detect. For example, pain may be a symptom while a rash may be a sign.
Tendinitis symptoms occur where the tendon attaches to a bone; and usually include:
- Pain - if the affected area is moved the pain worsens
- A feeling that the tendon is crackling or grating as it moves. This sensation is more common on examination.
- Swelling in the affected area
- The affected area may be hot and red
- A lump that develops along the tendon
If there is a rupture a gap may be felt in the line of the tendon and movement will be very difficult.
Causes of tendinitis
The condition is commonly caused by repetition of a particular movement over time. It can also be caused by a sudden injury. In the majority of cases, tendinitis develops in people whose jobs or hobbies involve repetitive movements; aggravating the tendons.
A tear in the tendon caused by an injury may cause swelling (inflammation).
Risk factors for tendinitis
A risk factor is something which increases the likelihood of developing a condition or disease. For example, obesity significantly raises the risk of developing diabetes type 2. Therefore, obesity is a risk factor for diabetes type 2.
Age - tendons become less flexible as we get older, making them more susceptible to injury.
Some jobs - if a person's job includes the following tasks their risk of developing tendinitis is higher:
- Repetitive movements
- Awkward positions
- Reaching overhead frequently
- Vibration
- Forceful exertion

Tennis elbow is caused by overuse of the forearm muscles.Sports - people who practice certain sports regularly are more likely to develop tendinitis, especially sports that involve repetitive movements, including:
- Running
- Tennis
- Swimming
- Basketball
- Golf
- Bowling
- Baseball
Diabetes - people with diabetes have higher risk of developing tendinitis. Experts are not sure why.
Rheumatoid arthritis - people with rheumatoid arthritis have a higher risk of developing tenosynovitis (when the sheath surrounding the tendon is inflamed).