Medi Services
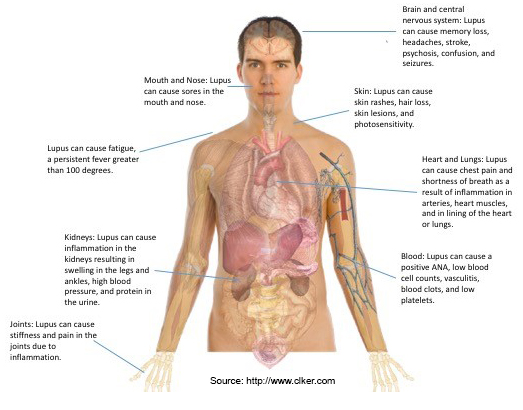
Lupus is a chronic inflammatory disease that occurs when your body's immune system attacks your own tissues and organs. Inflammation caused by lupus can affect many different body systems — including your joints, skin, kidneys, blood cells, brain, heart and lungs.
Lupus can be difficult to diagnose because its signs and symptoms often mimic those of other ailments. The most distinctive sign of lupus — a facial rash that resembles the wings of a butterfly unfolding across both cheeks — occurs in many but not all cases of lupus.
Some people are born with a tendency toward developing lupus, which may be triggered by infections, certain drugs or even sunlight. While there's no cure for lupus, treatments can help control symptoms.
No two cases of lupus are exactly alike. Signs and symptoms may come on suddenly or develop slowly, may be mild or severe, and may be temporary or permanent. Most people with lupus have mild disease characterized by episodes — called flares — when signs and symptoms get worse for a while, then improve or even disappear completely for a time.
The signs and symptoms of lupus that you experience will depend on which body systems are affected by the disease. The most common signs and symptoms include:
See your doctor if you develop an unexplained rash, ongoing fever, persistent aching or fatigue.
Lupus occurs when your immune system attacks healthy tissue in your body. It's likely that lupus results from a combination of your genetics and your environment. It appears that people with an inherited predisposition for lupus may develop the disease when they come into contact with something in the environment that can trigger lupus. The cause for lupus in most cases, however, is unknown. Some potential triggers include:
Factors that may increase your risk of lupus include:
Inflammation caused by lupus can affect many areas of your body, including your:
Having lupus also increases your risk of:

Diagnosing lupus is difficult because signs and symptoms vary considerably from person to person. Signs and symptoms of lupus may vary over time and overlap with those of many other disorders. No one test can diagnose lupus. The combination of blood and urine tests, signs and symptoms, and physical examination findings leads to the diagnosis.
Blood and urine tests may include:
If your doctor suspects that lupus is affecting your lungs or heart, he or she may suggest:
Lupus can harm your kidneys in many different ways, and treatments can vary, depending on the type of damage that occurs. In some cases, it's necessary to test a small sample of kidney tissue to determine what the best treatment might be. The sample can be obtained with a needle or through a small incision.
Treatment for lupus depends on your signs and symptoms. Determining whether your signs and symptoms should be treated and what medications to use requires a careful discussion of the benefits and risks with your doctor. As your signs and symptoms flare and subside, you and your doctor may find that you'll need to change medications or dosages. The medications most commonly used to control lupus include:
Take steps to care for your body if you have lupus. Simple measures can help you prevent lupus flares and, should they occur, better cope with the signs and symptoms you experience. Try to:
Sometimes alternative or complementary medicine may benefit people with lupus. However, these therapies are usually used with conventional medications. Discuss these treatments with your doctor before initiating them on your own. He or she can help you weigh the benefits and risks and tell you if the treatments will interfere with your current lupus medications.
Complementary and alternative treatments for lupus include:
If you have lupus, you're likely to have a range of painful feelings about your condition, from fear to extreme frustration. The challenges of living with lupus increase your risk of depression and related mental health problems, such as anxiety, stress and low self-esteem. To help you cope with lupus, try to:
Mayo clinic
Copyright © 2016 Seeking . All Rights Reserved . Design by Bluecircle
